Describe the Relationship Between Vaccination and Immunity
However when not everyone in a population can access vaccination herd immunity becomes vital in ensuring protection. Since the outbreak of COVID-19 the idea of herd immunity has entered the public vernacular as a way to reduce the.
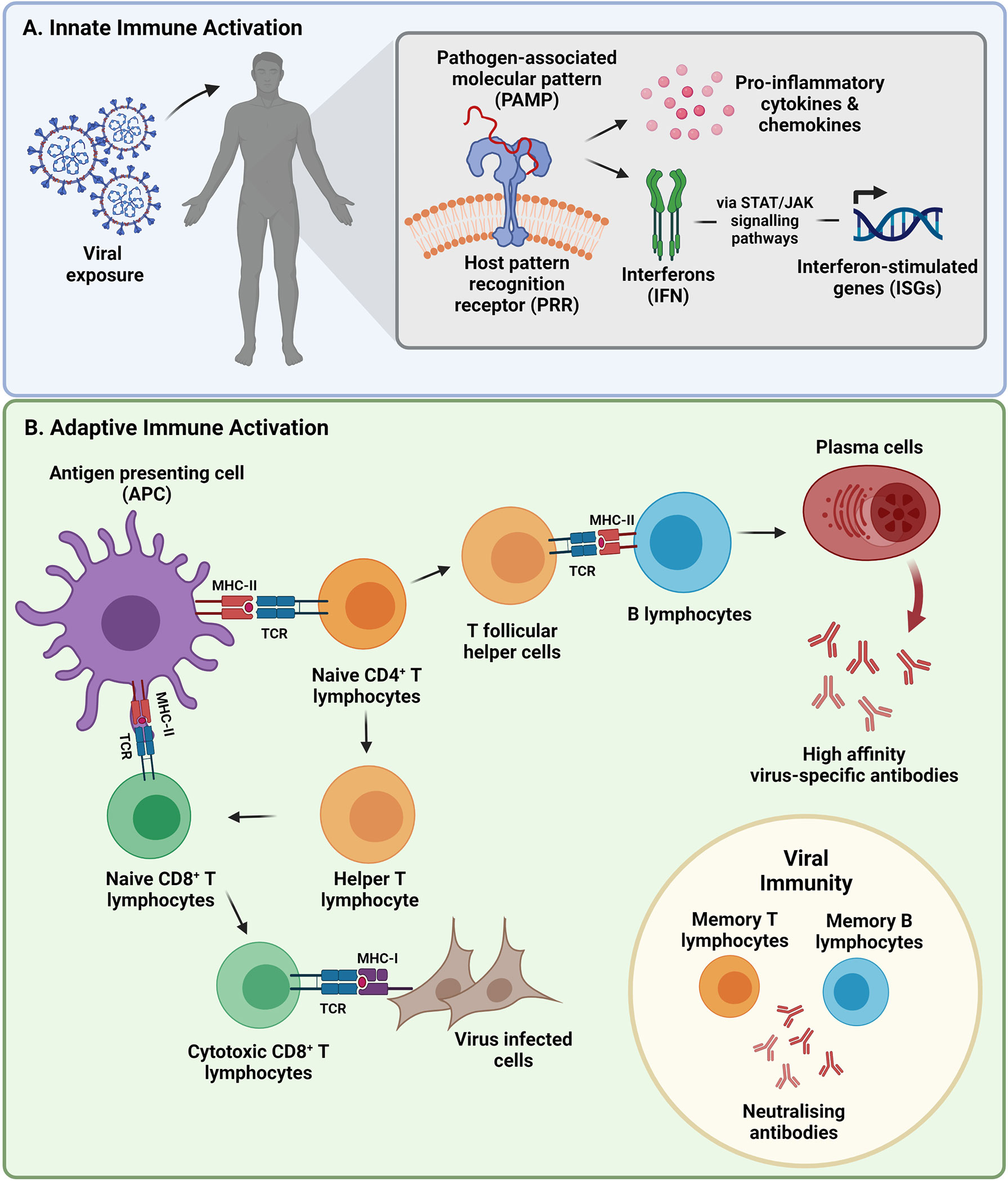
Frontiers Sars Cov 2 Variants Vaccines And Host Immunity Immunology
Vaccines train your immune system to create antibodies just as it does when its exposed to a disease.

. The relationship between nutritional status and immunity or between immunosenescence and vaccine efficacy is well documented 126 and it is known that the neonatal innate immune system which is biased against the production of proinflammatory cytokines impairs responses to many vaccines 127. However when scientists are designing vaccines they determine the smallest. It is true that natural infection almost always causes better immunity than vaccines.
For vaccine preventable disease outbreak. However there have been some recent conceptual developments in. Acquired immunity makes your immune system stronger.
However the difference between vaccination and natural infection is the price paid for immunity. Vaccines for example expose your immune system to small amounts of pathogens that wont make you sick. The antigens present on the surface of the pathogens act as markers that bind to the antibodies.
Active immunity is attained by exposure to a pathogen. Vaccines are needed to protect from SARS-CoV-2 the virus causing COVID-19. Vaccines that induce large quantities of high affinity virus-neutralizing antibodies may optimally prevent infection and avoid unfavorable effects.
The conventional idea of herd immunity is based on the relationship between the transmission dynamics of infectious agents and population immunity. Vaccines stimulate the innate immunity of host immunological defense mechanisms and induce the development of specific acquired immunity. The vaccines cannot give you COVID.
However the molecular mechanisms that underlie the impairment of. Herd immunity or contact immunity develops in the case of certain live vaccines eg OPV wherein the nonvaccinated individuals also develop immunity to the pathogen just by coming in contact with the vaccinated individual. Mechanisms of Vaccination and Immunity.
This paper suggests that vaccines are not a panacea in solving the pandemic of COVID-19 if the new variant provides a significant impact on transmissibility severity andor immunity. Dose When someone is exposed to viruses or bacteria naturally the dose is often larger so the immune response that develops will typically be greater as will the symptoms. Vaccination trials require precise clinical management complemented with de.
They can reduce the risk of severe illness from COVID. The Relationship Between Vaccines and Herd Immunity. Vaccination plays a key role in fighting against the pandemic of COVID-19 but it depends on the power of vaccines to resist the attack of new variants.
The differences between a vaccine and getting the disease naturally are the dose and the known time of exposure. Epub 2018 Apr 21. Some adverse events related to autoimmune responses have been reported such as idiopathic thrombocytopenic purpura and acute disseminated encephalomyelitis ADEM.
Rather than overwhelming the immune system vaccines help stimulate and strengthen it Immune systems need stimulation to develop well. Mathematical models of the spread and persistence of infection provide important insights into. The CDC estimates vaccines save 2 to 3 million lives per year.
Study finds correlation between vaccination rates disease immunity. An understanding of the relationship between the transmission dynamics of infectious agents and herd immunity provides a template for the design of effective control programmes based on mass immunization. Can someone please describe the relationship between immunity and vaccines.
Passive immunity is acquired when antibodies are introduced into the body from an external source usually through vaccines. Vaccinations are crucial in the fight against infections and viral spreads. This leads to the production of antibodies in the body.
IFN-γ production induced by the influenza vaccine antigens A H1N1 A H3N2 B Yamagata lineage and B Victoria lineage. Ad Safety is CDCs top priority and vaccination is the safest way to help build protection. Maricopa County most at-risk in US.
This review summarizes herd immunity focusing on conceptual developments with application to vaccination programs. Relationship between the frequency of influenza vaccination and cell-mediated immunity J Immunol Methods. In particular the influenza vaccine was administered to 21 adults during the 2015-2016 season.
Vaccination is a simple safe and effective way of protecting you against harmful diseases before you come into contact with them. Whereas immunity from disease often follows a single natural infection immunity from vaccines usually occurs only after several doses. Allergies may result from too little immune stimulation in our cleaner environments There is no evidence that vaccines can overload the immune system.
In this study we evaluated changes in cell-mediated immunity CMI with respect to the number of influenza vaccine doses. The immune system is designed to deal. Authors Naruhito Otani 1.
It uses your bodys natural defenses to build resistance to specific infections and makes your immune system stronger.

Comments
Post a Comment